NasalCrom for Neuroinflammation?
Cromolyn may help some Long Covid and ME sufferers with "brain fog." The nasal spray formulation reaches the cerebrospinal fluid and is available OTC in the US.
Mast cell stabilizer CROMOLYN may reduce neuroinflammation & improve cognitive function in some patients with Long Covid & ME/CFS. This article explains how.
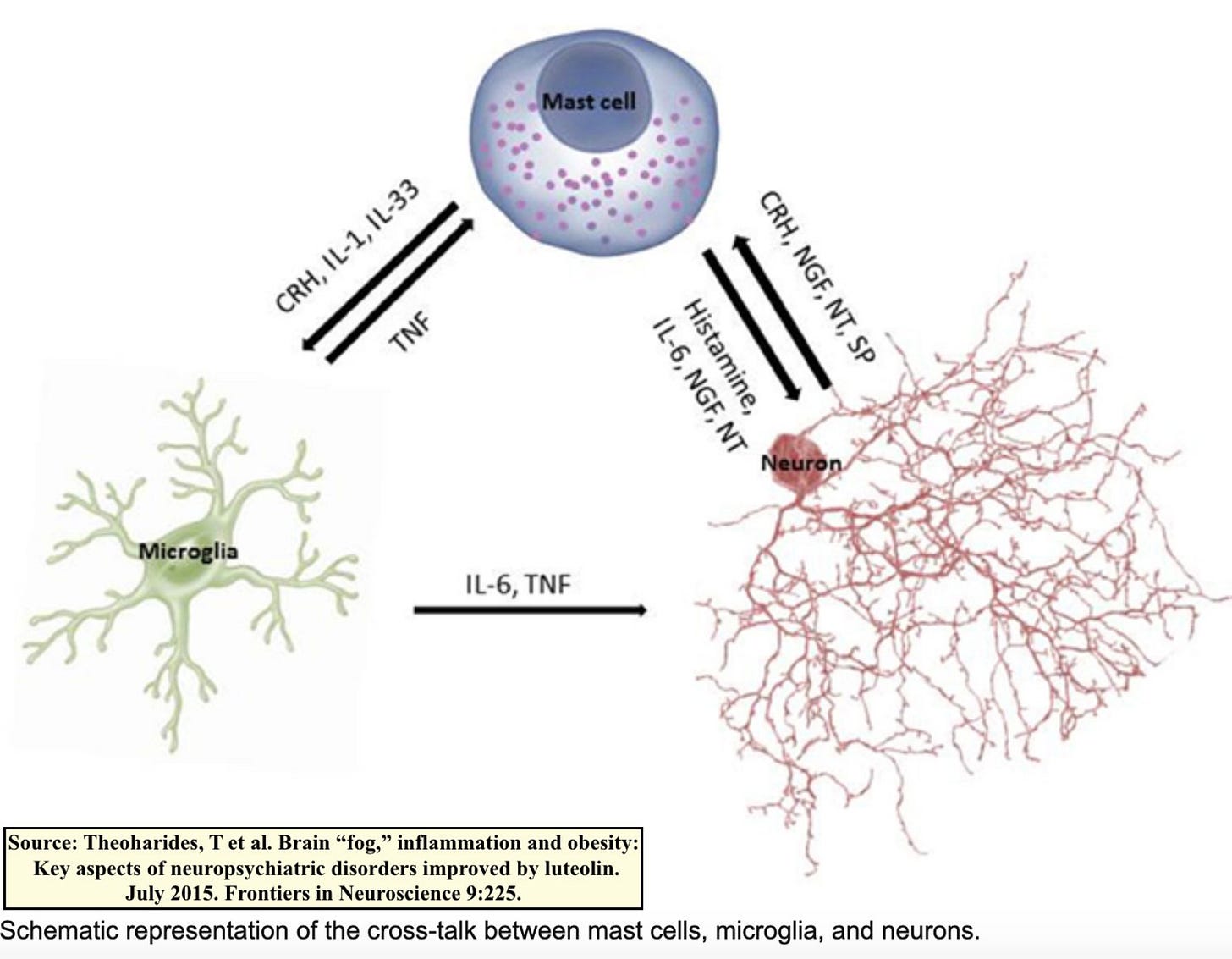
First, some background & context is necessary to understand how cromolyn works. In humans, mast cells release inflammatory molecules in response to pathogens which subsequently activate microglia, the primary neuroimmune cells in the central nervous system. Microglia make up ~5-20% of total brain cells. They secrete cytokines (notably TNF-α) & chemokines in response to changes:
This 2021 study found that microglial activation was the most common brain pathology found in deceased COVID patients (42.9%, or 79 in 184). 15% had microclots in brain tissue.
A June 2022 preprint presents in-vivo evidence of widespread neuroinflammation in two Long Covid sufferers. While this is a tiny sample size, authors explain that the very first two participants studied showed neuroinflammation, so they wanted to release their data ASAP. The two Long Covid patients were compared to three non-infected healthy controls. Disturbingly, PET imaging revealed that the neuroinflammation appeared even MORE widespread than in post-mortem brain tissue! Notably, the thalamus was affected, likely contributing to fatigue & cognitive disabilities.
Thus it appears that the following may occur for some with Long Covid (and perhaps those with ME/CFS considering similarities):
Infection -> mast cell activation -> microglial activation -> neuroinflammation
How can we attenuate this process? Several supplements show promise: intranasal cromolyn, luteolin and PEA. Today I review cromolyn.
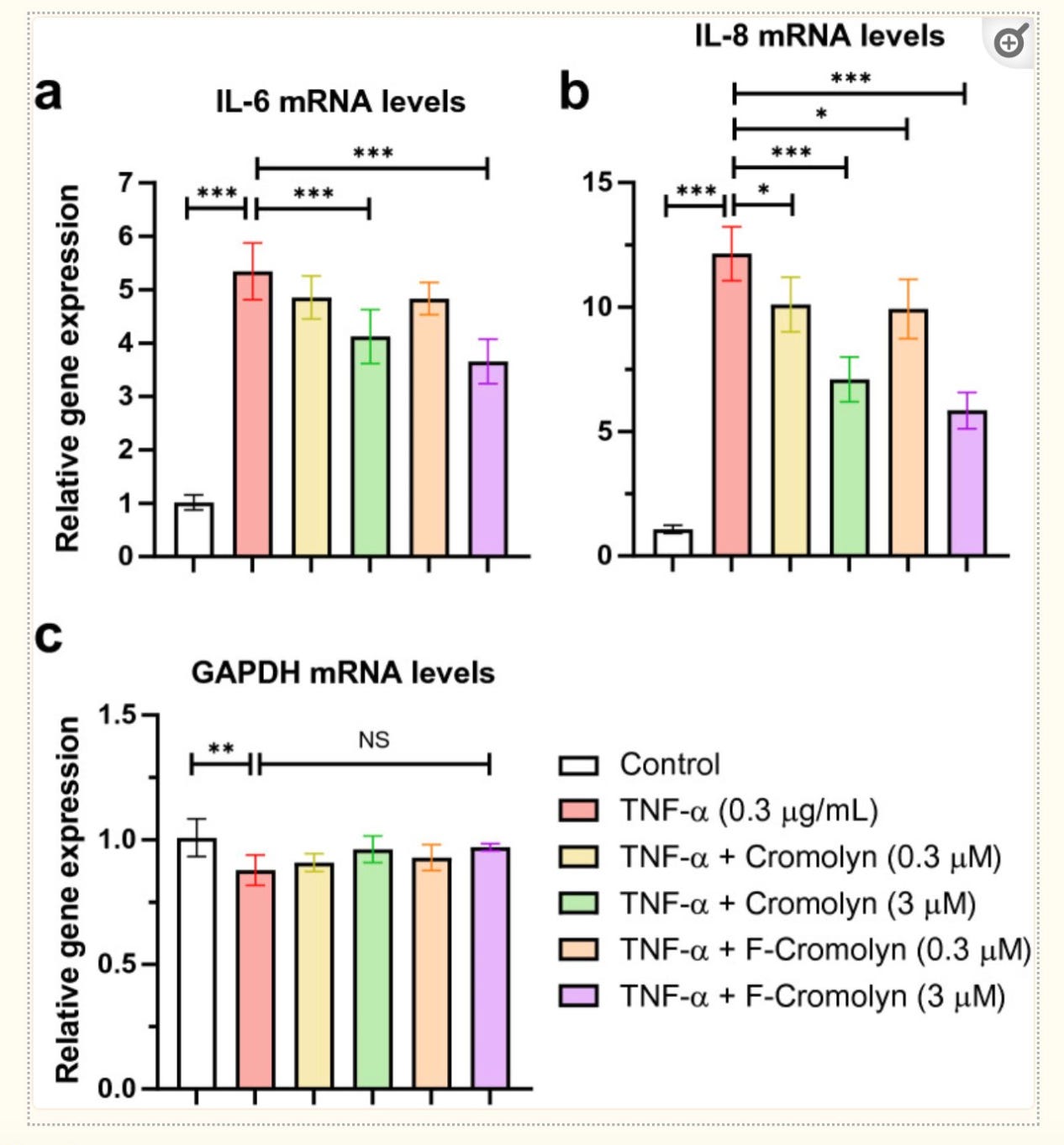
CROMOLYN inhibits sensitized mast cell degranulation which in theory should then tamp down on microglial & inflammatory cytokines. But does it? This 2021 study tested cromolyn's ability to dampen microglial pro-inflammatory responses in HMC3 microglia cell lines. The authors induced microglial activation by the inflammatory cytokine TNF-α and then compared the effects of cromolyn vs control. They found that indeed, cromolyn at 3 µM significantly inhibited inflammatory cytokines & chemokines secreted by microglia:
Not only did cromolyn reduce levels of IFN-y, IL-6, IL-1ß & IL-8 by 47%, 40.5%, 49.3%, & 25.8%, respectively, but the drug also significantly reduced their relative gene expression and prevented HMC3 microglia cell death induced by TNF-α in a concentration-dependent manner:
A 2017 mouse study found likewise reductions in inflammatory cytokines by cromolyn. Authors concluded: "Interactions between mast cells and microglia could constitute a new and unique therapeutic target for CNS immune inflammation-related diseases.” Soon thereafter, a 2018 mouse study published in Nature concluded that cromolyn induced a "neuroprotective microglial activation state favoring Aβ phagocytosis versus a pro-neuroinflammatory state." This also aligns with the results from the aforementioned 2021 study.
Several human trials are currently investigating the neuroprotective and anti-inflammatory effects of cromolyn in covid pneumonia and Alzheimer's disease. Before the Alzheimer's trial began, a study was performed to investigate the pharmacokinetics, safety & tolerability of inhaled cromolyn. The study showed average maximum concentrations in the cerebrospinal fluid of 0.24 ± 0.08 ng/ml & 0.34 ± 0.17 ng/ml after 17 & 34 mg inhaled doses, respectively. Unfortunately, this converts to a significantly lower concentration than the 0.3 µM & 3 µM tested in vitro. Nevertheless, authors concluded: “The concentrations of cromolyn…observed in the CSF are considered sufficient to titrate the estimated daily amyloid production and the associated inflammatory response in patients with AD.”
Anecdotally, some Long Covid sufferers have reported significant cognitive benefits with NasalCrom, an OTC cromolyn nasal spray which can be purchased from most drug stores in the United States. It is also available for online purchase in Europe here. Oral cromolyn is available by prescription only in Europe, but the nasal spray shows better systemic and CSF absorption and thus looks to be a more promising route of administration for neuroinflammation.
A few facts on NasalCrom:
It is safe in children as young as 2 years old.
Its onset of action is typically 1-2 weeks.
Take daily every 4-6 hrs for at least 2-4 weeks for full effects.
It is well-tolerated with very few known drug interactions.
It is relatively inexpensive and low-risk medication to trial for those with cognitive dysfunction or post-covid “brain fog.”






How long should someone use the nasal spray after a positive Covid test?
Hi, thank you so much for your work! I tried to find any survey result for supplements… did you do a survey for they? I don’t recall. I’m looking for info on Quercitin, specifically. And info on how to find a “reliable” supplement company!
I don’t have a Twitter account (try to keep online presence to a bare minimum) but I saw some posts this spring about your health and felt so bad for you. I wanted to share some thoughts that might spark some idea… though you seemingly think of everything. I was pretty bad around Christmas, started NK/SP per your writings (I don’t like to experiment randomly and strongly prefer scientific evidence- just not much exists, I think I have similar philosophy to you) and began to feel better over the next couple months. But then May was pretty brutal, and I didn’t know why. Then it occurred to me I had started Claritin around the same time as NK/SP because I had seasonal allergies for 20 years (though they mysteriously disappeared the year the pandemic began. Didn’t know what to make of that but working in the ER, I was too busy and freaked out to give it much thought). I try hard to only change one variable at a time but this OTC Claritin I’d taken every year for two decades became an afterthought. And I realized I stopped it in May because I was feeling better and wanted to cut out extraneous pills. Then I realized after reading much more about it, I really fit the profile for MCAS. I resumed the Claritin, now doing a bit better on H1/2 blockers. I’d tried that combo for a month a year ago without effect. But then I realized maybe I needed to handle the microclots first/together with NK/SP in order for antihistamines to have an effect.
Just wondering and hoping if this hypothesis /anecdote might help you. It’s hard to stay scientific without simple biomarkers or definitive mechanism, but you inspire me to try my best to be rational about what I do.